Series of articles from Dr Paul Batman PhD.
Remember you can use these articles for your own social media and websites. If you need the word copies just ask!
What’s on TV tonight?
Up to 20% of Australians over 20 years of age have metabolic syndrome defined as an increase in abdominal obesity, glucose intolerance, increased fat in the blood, hypertension and high blood pressure and insulin resistance similarly seen in diabetes.

Prolonged TV watching has been associated with the reduced activity of a special transporter whose job is to transport any glucose from the blood into the muscle. If the enzyme malfunctions the result is an increase in the amount of sugar in the blood and could potentially lead to diabetes or other metabolic conditions.
The level of cardiovascular risk in children has also increased dramatically over the past 20 years, which can lead to an increased risk in later life.
Previously it was suggested that diet and lack of exercise were the key determinants of this epidemic.
Researchers have focused on sedentary behaviour and prolonged TV watching as a possible cause with a significant association found between TV watching, sedentary behaviour and increased cardiovascular risk in adolescents.
Adolescents have been accused of substituting movement with more sedentary behaviour such as TV watching, gaming, computer use, social networking, sitting to and from school, sitting at lunch time, sitting at dinner etc. Prolonged sitting while watching TV has been linked to obesity, metabolic syndrome.
A second influence that is associated with TV watching is the increased opportunity for snacking, increased consumption of energy dense foods, decreased consumption of fruit and vegetables and general increase in energy intake.
In addition to TV watching gaming is rapidly becoming a family activity. In a study reported by Bond University in Australia a survey or 1252 families revealed that 95% of those households with children under 18 years of age had at least one gaming device with more than 80% of parents admitting to playing video games.
From a cohort of females in a Nurse’s Health study it was found that 2 hours per day of TV viewing was associated with a 23% increase in obesity and a 14% increase in diabetes, while sitting at work was associated with a 9% increase in obesity and a 7% increase in diabetes. Conversely, standing or walking around at home for 2 hours per day reduced the prevalence of obesity by 9% and 12% in diabetes.
It apparently takes only 4 hours of continuous sitting while watching TV for muscles to get into a sleep mode where the genes recruited to regulate glucose and fat clearance begin to shut down.
So get up and move around every commercial break or stand while watching your favourite show….
Could it be about where we live?

Why is it that there are pockets in the world where some people seem to live forever!
National Geographic writer Dan Buettner and a team of researchers travelled the world to identify the specific pockets where people live a higher quality of life than the norm.
From their observations they identified the Five (5) Blue Zones.
“The Blue Zones are places where the inhabitants have the greatest life expectancy and live past 100 years more than anywhere else in the world. They identified Okinawa in Japan, Sardinia in Italy, Loma Linda in California, Nicoya in Costa Rica and Ikaria in Greece as places on earth where people live to 100 years ten times more often than the equivalent in the United States.”
Buttener identified six areas where lifestyle choices affected the longevity of the inhabitants of these regions. These centres include: community, workplace, social, financial, domestic and self.
Two of the blue zone areas that have been studies most widely include the Ikaria islands and Okinawa .
Ikaria
Ikaria lies in the Aegean Sea between the Greek Islands of Samos and Mykonos and has reportedly one of the longest life expectancies in the world.
One of the main reasons for its people’s longevity is the increased physical activity level of the islands’ inhabitants. Approximately 90% of the males and 70% of the females reportedly take part in daily physical activity, mainly occupational.
Ikaria males live longer than any other males throughout the world. These percentages far exceed those of the other Greek Islands where 50% of males and 25% of females are reportedly active on a daily basis.
More than 60% of the Ikaria inhabitants over the age of 90 years report they were still physically active on a daily basis. Very few males and females were current smokers although a large proportion had smoked at some stage in their lives.
The Ikaria people eat a Mediterranean diet high in vegetables, fruit and salads and were not influenced by western style foods or diets. Other characteristics that contributed to a long life included: avoidance of smoking, midday naps, social engagement and family coherence.
Okinawa
The Okinawan centenarian study, which has been ongoing since 1975 ranks Okinawa as the number one location in the world for longest life expectance and also world’s longest health expectancy. When compared to the USA (which represents western lifestyle) only 18 per 100,000 people suffer from cardiovascular disease, 97/100,000 from cancer, 35/100,000 from stroke and 335/100,000 for all cause mortality.
The USA, which is ranked 18 in world, presents with 100/100,000 for cardiovascular disease, 132/100,000 for cancer, 38/100,000 for stroke and 520/100,000 for all cause mortality.
These numbers are amplified by 50 per 100,000 people reaching 100 years of age in Okinawa compared to 10-20 people per 100,000 reaching the same age in the USA.
The longevity of Okinawans has been attributed to genetics, caloric restriction and metabolic damage, cardiovascular health, increased physical activity, stress reduction lifestyle and hormonal profile. Perhaps the two characteristics that continual to appear in other studies are caloric restriction and physical activity.
Typically Okinawans consume a low calorie, low glycemic and caloric control diet. They practice a cultural habit known as “hara hachi-bu” where they only eat until their stomach is 80% full. This is said to reduce the formation of free radicals generated by metabolizing food into energy. The free radical production has the potential to damage organs over a long period of time.
Okinawans keep active through domestic activities, occupational activities and general lifestyle prescriptions rather than formal exercise interventions.
Okinawans also demonstrate lower levels of osteoporosis possible due to the low to moderate levels of weight bearing activities performed as well as a diet high in calcium.
So if we want to live to be 100 years old we need to pack our bags, buy a plane ticket (making sure we move constantly in our seat or buy a business or premium economy class ticket) and move to a Blue Zone!!
Do I have to do everything Mum tells me to do?
Remember when our mothers told you could not go swimming immediately after we ate a meal? Sometimes we had to wait for up to 30 minutes before taking the plunge.

Sadly she was wrong!
Over the past 40 years there has been a frightening increase in the number of people with diabetes with a sedentary lifestyle identified as the cornerstone of this increase.
As a result some of us could develop diabetes while the majority might just experience high blood sugar levels or hyperglycaemia. Two thirds of all people with pre diabetes or hyperglycaemia will eventually develop full diabetes.
It is important for us to control our blood sugar levels and reduce our chances of developing diabetes.
The mechanism for the control of high blood sugar starts with the eating of the meal, which is followed by an increase in blood sugar in the bloodstream. To combat this increase the pancreas releases insulin, which then provides passage for the blood sugar into the muscles and organs thereby reducing and controlling blood sugar.
The greatest peak in blood sugar doesn’t occur immediately after the meal. The main surge occurs about 60 minutes after the meal. At this time there is a significant increase in the release of insulin and the blood sugar is initially shuttled in the large muscles of the thigh, buttocks and trunk.
The sugar delivery system is designed to provide the muscles and organs with fuel for energy. This system is designed to allow the body to move continuously after eating. It is similar to when we fill up our car at the service station. We pump the petrol into the car to provide the energy for the engine to drive the car.
If we have a normal lunch while we are at work and then go back to our desk, our elevated blood sugar remains unused moving around our blood vessels.
The sedentary muscles have no need for the increased blood sugar and by remaining dormant they don’t assist insulin with the movement of the blood sugar into the muscle.
The increased blood sugar plays havoc with the insulin receptors on the muscles and organs. If eventually high blood sugar becomes chronic the insulin receptors become resistant to insulin causing a significant amount of surplus sugar to remain in the blood eventually leading to pre diabetes or diabetes.
Think how many times during our normal working week that we have got up and moved immediately after any of our meals.
The body’s cellular mechanisms were not designed for sitting. Without some sort of movement to relocate the blood sugar most of it will simply hang around in the blood until it finds its way into the muscle, organs or fat cells with the help of insulin. This increases the reliance on insulin and decreases the role of the muscle in removing blood sugar.
If we crank up our large muscles after a meal there is an increase in the movement of the blood sugar into the muscles, reducing the blood sugar spike and the amount of insulin required to eventually move the blood sugar into the muscle or organs.
To confirm this theory, a study measured blood sugar and N.E.A.T. (non exercise activity thermogenesis) every second before and after subjects consumed a meal. The conclusion from the mountain of data collected revealed that after the subjects ate the meal there was huge spike in blood sugar for approximately two hours post meal.
Those subjects who walked very slowly for 15 minutes immediately after their meal were found to have 50% less blood sugar swirling around in the blood vessels.
So the bottom line is don’t take any notice of your mother.
As soon as we finish our meal we should get up on our feet and move around for 5-10 minutes to help our large muscles disperse the accumulated blood sugar without relying on a huge increase in insulin secretion.
We should spend 50% of our lunchtime eating our meal and the remaining time going for a walk before we go back to our desk.
If we are close to a pool or water we should feel free to dive in and splash around..
What would happen if you ate an additional 1,000 Kcal per day for 8 weeks?
The answer has always been that our weight would increase simply because we ate too much food. However, we know that not everyone gains weight when they eat the same amount of food.
There has always been a question as to why some people appear to be able to eat everything and not put on weight while others only have to look at food and the pounds or kilograms stack on!!
One of the first studies to examine overfeeding was conducted in 1990 by Dr Claude Bouchard who overfed 12 pairs of male twins an additional 1,000 Kcals per day for 6 days (the seventh day they could eat anything) for 14 weeks. In other words they were feed 84,000 additional Kcals over three months!!
The weight gain in this study ranged from 4 kilograms to a high of 14 kilograms. The researchers found that some people had bodies that were susceptible to weight gain while others appeared more efficient at using the additional Kcal.
Where did the missing Kcal go given that this cohort of subjects lived in the same environment under the same feeding conditions?
In an attempt to answer this question Dr James Levine overfed a group of sedentary subjects from all walks of life that did not participate in any fitness training programs. After determining the number of Kcal required to maintain their normal body weight, the subjects were overfed an additional 1,000 Kcal per day for 8 weeks, while still continuing with their normal daily activities.
This group ate an additional 56,000 Kcal over the 8 weeks of the study.
Again the results showed that some subjects put on up to 7 kilograms while others appeared not to put any weight at all, while the remaining subjects were somewhere in the middle.
Again the question was asked “ Why did some put on significant amounts of weight while others barely gained any weight” None of these subjects were exercising in any form and only performed their normal daily activities.
So what is the answer? Is it that they really do have a slow metabolism or are just big boned?
Those subjects who put on the most weight were those who remained stationary by sitting or lying down for the majority of their day.
The weight gainers sat on average an additional 2.5 hours per day than those who controlled their weight gain.
Those who controlled their weight gain walked more, stood more and fidgeted more to the tune of an additional 350 Kcal per day. They tended to be more habitually active while eating the additional Kcal.
If an average person expended an additional 350 Kcal per day they have the potential to lose 18 kilograms in 12 months.
These studies tell us that putting on weight is not just about the amount of food that we eat.
Those who could control their weight gain were those who lived their life with greater movement, not necessarily by going to the gym but by performing more active living movements in the home, at work, using active transport, standing and walking.
The weight gain was not only associated with the additional food consumed but the amount of NEAT (Non exercise activity thermogenesis)/NEPA work the subjects expended during their day
So the answer as to why some people gain weight and others don’t given that they might consume similar amounts of food could lie in the daily incidental movements that they perform.
Given that over the past 50 years we have been robbed of over 150 Kcal per day by labour saving devices and changes in our work environments the increase in obesity rates could be partly accounted for by the decreasing amount of NEAT/NEPA.
We know that daily energy expenditure is divided into basal metabolic rate, thermic affect of food and activity thermogenesis. Activity thermogenesis is divided into exercise thermogenesis and non-exercise thermogenesis (NEAT).
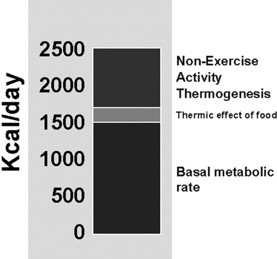 The NEAT/NEPA is the section where the greatest amount of energy expenditure is potentially possible and the one that can be manipulated the most.
The NEAT/NEPA is the section where the greatest amount of energy expenditure is potentially possible and the one that can be manipulated the most.
If we find ourselves in a situation where we are eating more than we normally do, few need to find ways of expending additional energy by increasing our NEAT/NEPA.
What would happen if you ate an additional 1,000 Kcal per day for 8 weeks?
The answer has always been that our weight would increase simply because we ate too much food. However, we know that not everyone gains weight when they eat the same amount of food.
There has always been a question as to why some people appear to be able to eat everything and not put on weight while others only have to look at food and the pounds or kilograms stack on!!
One of the first studies to examine overfeeding was conducted in 1990 by Dr Claude Bouchard who overfed 12 pairs of male twins an additional 1,000 Kcals per day for 6 days (the seventh day they could eat anything) for 14 weeks. In other words they were feed 84,000 additional Kcals over three months!!
The weight gain in this study ranged from 4 kilograms to a high of 14 kilograms. The researchers found that some people had bodies that were susceptible to weight gain while others appeared more efficient at using the additional Kcal.
Where did the missing Kcal go given that this cohort of subjects lived in the same environment under the same feeding conditions?
In an attempt to answer this question Dr James Levine overfed a group of sedentary subjects from all walks of life that did not participate in any fitness training programs. After determining the number of Kcal required to maintain their normal body weight, the subjects were overfed an additional 1,000 Kcal per day for 8 weeks, while still continuing with their normal daily activities.
This group ate an additional 56,000 Kcal over the 8 weeks of the study.
Again the results showed that some subjects put on up to 7 kilograms while others appeared not to put any weight at all, while the remaining subjects were somewhere in the middle.
Again the question was asked “ Why did some put on significant amounts of weight while others barely gained any weight” None of these subjects were exercising in any form and only performed their normal daily activities.
So what is the answer? Is it that they really do have a slow metabolism or are just big boned?
Those subjects who put on the most weight were those who remained stationary by sitting or lying down for the majority of their day.
The weight gainers sat on average an additional 2.5 hours per day than those who controlled their weight gain.
Those who controlled their weight gain walked more, stood more and fidgeted more to the tune of an additional 350 Kcal per day. They tended to be more habitually active while eating the additional Kcal.
If an average person expended an additional 350 Kcal per day they have the potential to lose 18 kilograms in 12 months.
These studies tell us that putting on weight is not just about the amount of food that we eat.
Those who could control their weight gain were those who lived their life with greater movement, not necessarily by going to the gym but by performing more active living movements in the home, at work, using active transport, standing and walking.
The weight gain was not only associated with the additional food consumed but the amount of NEAT (Non exercise activity thermogenesis)/NEPA work the subjects expended during their day
So the answer as to why some people gain weight and others don’t given that they might consume similar amounts of food could lie in the daily incidental movements that they perform.
Given that over the past 50 years we have been robbed of over 150 Kcal per day by labour saving devices and changes in our work environments the increase in obesity rates could be partly accounted for by the decreasing amount of NEAT/NEPA.
We know that daily energy expenditure is divided into basal metabolic rate, thermic affect of food and activity thermogenesis. Activity thermogenesis is divided into exercise thermogenesis and non-exercise thermogenesis (NEAT).
The NEAT/NEPA is the section where the greatest amount of energy expenditure is potentially possible and the one that can be manipulated the most.
If we find ourselves in a situation where we are eating more than we normally do, few need to find ways of expending additional energy by increasing our NEAT/NEPA.
It can’t be that simple….can it?
We now know that sedentary behaviour as measured by “sitting time” is now the “New Smoking” and a major health issue. We have been told that to overcome some of the serious side effects of sitting we have to find more time to stand during our day. The recommendation is to stand for as along as possible when the opportunity presents itself. This is now being challenged.
Information on space flight and long-term bed rest now being revisited has provided a new and possibly more manageable approach to standing.
You might ask what bed rest, space and sedentary behaviour have in common. The answer is that they all produce similar physiological long-term effects.
Astronauts returning to earth after missions all present with similar symptoms including muscle weakness, bone loss, fainting and calcium loss. These conditions were termed “Space Hangovers”.
If an astronaut spends less than 30 days in space in a zero gravity environment they generally require significant time back on earth to recover, with 6 months of zero gravity potentially take up to two years of recovery time!!
Even more dramatic is the astronaut who lives in zero gravity for longer than 14 months. This space traveller could take up to 10-20 years to recover!!
Anyone volunteering to go to Mars?
NASA attempted to overcome these physical problems by instituting an exercise program in space. Positive effects were noted from the space exercise program but they were short lived. The detrimental effects soon came back. This led the NASA experts to state that physical exercise had only a 50% success rate in maintaining muscle mass, bone health and cardiovascular health while in space.
In an attempt to replicate space conditions NASA has spent many years conducting bed rest studies with subjects lying on their back with their head lower than their body (6 degrees).
Dr Joan Vernakos , a senior researcher at NASA has coined the term “Gravity Deprivation Syndrome”, which is caused by continuous bed rest, space flight or a sedentary lifestyle.
As little as 4 days of bed rest can be enough to initiate gravity deprivation syndrome.
This syndrome is initially seen as a reduction in blood volume, an increase in hypostatic hypotension and increased loss of calcium in the urine. These changes occur quite rapidly.
It is interesting to note that hospitals now insist that patients get out of bed as soon as possible after surgery to ensure that the side effects of bed rest are attenuated.
In a study that compared walking upon rising from bed to simply standing at the end of the bed without any walking the results might surprise you.
It was reported that standing without walking was more effective in regulating blood pressure and the restoration of blood pressure.
One of the main reasons given for this interesting observation was that upon standing the heart has to pump harder to push blood from the lower body up the head without the help of the muscles of the leg assisting with the movement.
This is in contrast to walking where the strain on the heart is reduced somewhat as the vessels of the leg muscles receive less stimulation as the muscles contract and assist with the pumping action. The more frequent sitting and standing provide a better stimulus for the regulation of blood pressure.
In a Japanese study subjects aged between 25-55 years old were the first to show that total bed rest (no getting up at all) for 4 to 84 days resulted in an increase in the symptoms of advanced ageing.
The question now becomes “does standing up more often provide a greater stimulus than continual standing and walking?”
The answer is standing up more often is what matters, not how long we stand.
When we rise from a squatting position there is a significant shift in fluids, blood volume and the release of hormones with large hip and leg muscles also contracting. Enzymes responsible for transporting fat to the muscles are also actively stimulated.
The standing movement also stimulates vascular reflexes in the blood vessels that change their diameter ensuring an adequate blood supply to the brain.
Lying on our back for long periods can also rob our brain of the blood flow that it requires to function normally. It is in this position that the blood vessels reflex become impaired.
Dr Vernakis states that almost every nerve in our body is innervated when we stand.
If we were stand for 32 minutes at one time our body would have one initial shock to get us started for the 32 minute standing bout, after which time our body would tolerate the movement and adjust to ensure we maintain our upright posture.
If on the other hand we stood up for less than one minute x 32 times per day our body would read that as 32 new stimuli that it would have to contend with, causing 32 different significant physiological reactions.
Dr Vernakis recommends standing from a sitting position every 15 minutes of our workday. This can be for as little as a minute or less for a total of 32 standing movements. It can be that simple!
Could TELOMERES be the answer to ageing and chronic disease?
In the nucleus of each cell, our genes are stacked into DNA molecules tightly packed into thread-like structures called chromosomes surrounded by specific proteins that support its structure.
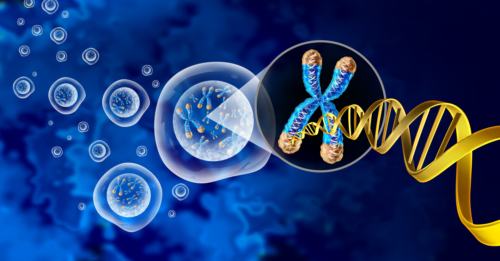
The shortening of the telomere is a reflection of the number of times the cell has divided. When they get too short and the cell can no longer divide, it becomes inactive, “old” or dies. This shortening process is associated with ageing, cancer and a higher risk of death. Telomeres are like a time bomb ready to go off at any time!
Cells can normally divide only about 50 to 70 times, with telomeres getting progressively shorter until the cells become old or dies.
Without telomeres the genes essential for life would get shorter each time a cell divides. Telomeres allow cells to divide without losing genes. Cell division is necessary for growing new skin, blood, bone, and other cells.
Telomerase is the enzyme that ignites many of these reactions and remains active in sperm and eggs, which are passed from one generation to the next.
If reproductive cells did not have telomerase to maintain the length of their telomeres, any organism with these cells would soon become extinct.
As a cell begins to become cancerous, it divides more often, and its telomeres become very short. If the telomere gets too short, the cell may die. Often times, these cells escape death by making more telomerase enzyme, which prevents the telomeres from getting even shorter.
Successful ageing requires an ability to balance damage with repair of cells. When the damage to the cell overcomes the repairing of the cell subsequent long-term degeneration will occur subjecting us to Alzheimer disease, cardiovascular disease, Type II diabetes and Sarcopenia.
Many cancers present with shortened telomeres, including pancreatic, bone, prostate, bladder, lung, kidney, and head and neck.
Geneticist Richard Cawthon from the University of Utah found shorter telomeres were associated with shorter lives. In a sample of people older than 60 years, those with shorter telomeres were three times more likely to die from heart disease and eight times more likely to die from infectious disease.
Without telomeres, chromosome ends could fuse together and corrupt the cell’s genetic blueprint possibly causing malfunctions or cell death. As broken DNA is dangerous, a cell will sense and repair the damaged chromosomes. Without telomeres, the ends of chromosomes would look like broken DNA. The cell would try to repair something that wasn’t broken forcing the cell from dividing and eventually dying.
Cawthon’s study found that people with longer telomeres lived an average of five years longer than those with shorter telomeres. He suggested that increasing the length of telomeres in people with shorter ones could increase the lifespan by approximately five years.
A major cause of ageing is “oxidative stress.”
Oxidative stress is the damage to DNA, proteins, and lipids (fats) caused by oxidants, which are highly reactive substances containing oxygen.
The free radicals that are produced in combination with the consumption of alcohol and cigarettes can result in inflammation and infection, all of which has an impact on shortening the telomere.
We know that if people who have a low fitness level, who are obese, are older or are suffering from a chronic disease undertake high intensity exercise have the potential for the unregulated production of free radicals (ROS) that can have serious side effects, particularly on the cell membrane.
Several studies have reported a positive association between physical activity and telomere length. Active individuals have longer telomeres in their immune cells compared to sedentary individuals, with differences in telomere length equating up to approximately 10 years difference in biological age.
Some studies have reported that moderately active individuals have longer telomeres compared to both sedentary and extremely active individuals.
One study reported that 50–70 year-old individuals in both the lowest < 990 Kcal/wk and highest energy expenditure > 3541 Kcal/wk had shorter telomeres than individuals in the middle group who expended between 991– 2340 Kcal/wk, even when controlling for age, gender, and body weight.
Moderate intensity physical activity (3-6 METs) is more likely do not cause skeletal muscle damage, does not result in an excess ROS and inflammation and does not shorten telomeres. As a consequence moderate intensity activity would appear to at least maintain or more likely increase telomere length with age.
The available research data supports physical activity in combination with stress reduction and dietary modifications over a long period can slow cellular ageing and improve health as indicated by reduced telomere shortening.
Are you using the right type of muscle fibre?
Remember when..
Remember a few years ago when information was released that made us stop and examine how we were training our abdominals. We were told that the abdominals can be trained more effectively by planking positions and holding the contraction for up to 30 seconds, rather than continually performing hundreds of crunches or variations.
One of the main reasons for this insightful information was the realization that the main function of the core was stability and to train the stabilizers we needed to focus on less intense contractions but held for a long period of time.
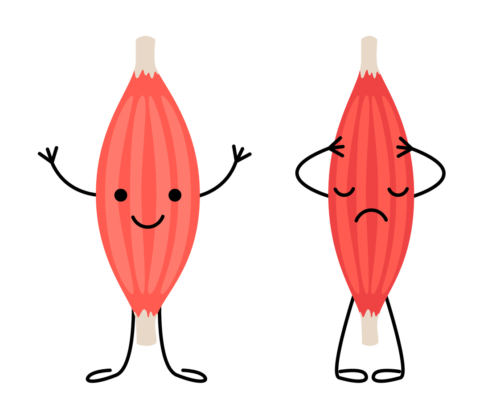
It makes sense now that the deep muscles of the spine are active for long periods stabilizing the trunk and with what we know about specificity we can rationalize that to train these key muscles requires the recruitment of slow twitch muscle fibres (Type 1). These fibres are designed to produce low force contractions sometimes lower than 30% of maximum contraction often with no obvious movements.
The same principle can now be applied to other types of physical activity.
If we are at the gym and training at high intensity with fast movements the typical muscle fibre recruited is fast twitch or Type 2 muscle fibres. These muscle fibres are used intermittently during your day when fast or strong muscle contractions are needed.
The muscle fibres that are active throughout our day maintaining posture and allowing us to move continuously are slow twitch or Type 1 fibres.
Stabilizer muscles consist of a greater proportion of slow twitch or Type 1 fibres. If these muscle fibres are critical to our ability to fight gravity then surely they must play a significant role in balance, direction and movement. For improvements to occur, we need to move more to increase the fibre’s mitochondria (powerhouse of cell), increase its oxygen ability, increase its blood flow and increase its resistance to fatigue.
Higher intensity exercise is great for increasing our VO2 max (maximum oxygen capability) and improving our aerobic fitness. It creates significant overload on our heart’s ability to pump blood through both stroke volume and cardiac output increases and recruits fast twitch muscle fibres. But its limitation is its inability to recruit significant numbers of slow twitch muscle fibres that we have previously identified as important for keeping us upright, balancing our body and moving in a multitude of directions.
Slow twitch muscle fibres perform at their best when they are recruited for long periods of time without being turned off. If we have a desk job and religiously go to the gym and do our 60 minutes high intensity workout, the
reality is that we might not be activating the type of muscle fibres that are responsible for most of the movements performed in a day. Apparently there is very little carryover, leading to us to become an “active couch potato”.
The principle of specificity clearly states that the responses we receive from training or exercising are directly related to the dose of intensity, frequency and duration that we prescribe.
If we are to recruit the important slow twitch muscle fibres in order to improve our health, we have to make time to activate them outside of the gym or fitness environment.
Stabilizers need to be active for as much of the day as possible.
It is the small, brief, continuous, low force producing intermittent muscle contractions that we use in our natural everyday activities that are the mainstays to a healthy lifestyle.
These low force producing everyday movements that recruit slow twitch muscle fibres are integral to the control of various fat metabolizing enzymes, control of blood sugar, reduction in blood pressure, reducing LDL or bad cholesterol and weight control.
Don’t think for a minute I am saying that high intensity exercise is bad. Quite the contrary, I am saying it has its place if we are looking to improve our aerobic fitness (after you have progressed to it) and weight maintenance.
We should start thinking outside of the box and not beat ourselves up if we don’t like high intensity exercise, as there are plenty of benefits for us by substituting our sedentary activities with just low to moderate movements.
For a start try this: Take a movement inventory of what your day comprises on an “hour by hour” basis. Look at the times when you are sitting at home, at work, transport to and from work and during your leisure time and substitute these inactive minutes with active minutes… you might be surprised with the results!!!
What is the real truth? You can’t argue with numbers….
To discourage us from eating the wrong foods we are often told what exercise would be required to burn the food item off. We have been told that if we eat that chocolate bar we will have to go to the gym and work for at least an hour at high intensity to work it off. Conversely we are also told that working out at the gym or in the park at high intensity is the best method for weight reduction.
It makes sense that the harder we work the more kilojoules we will burn, and it has to be correct because we see it on television!!
The question is how do we measure these claims?
The American College of Sports Medicine (ACSM) is one of the most revered professional colleges on the planet. They have led the exercise science revolution for over 60 years. In recent years they have promoted a series of calculations to measure our energy expenditure and to answer these questions.
I would like to present a case study with calculations and numbers that might help us answer these questions and frighten us with the answers.
Just because I mentioned calculations and numbers PLEASE don’t leave me now as we are just getting to best part….. work with me!!
Say Hi to Peter
I would like to introduce you to my friend Peter.
Peter is a 45 years old high-powered executive who has body fat percentage of 37%. He weighs 110 kilograms and is 173 cm tall and has a BMI of 34 kg.m-2 classifying him as obese. Peter has increased his body weight over the past three years mainly due to his sedentary lifestyle. Peter does no exercise at all and eats at restaurants for lunch on most days. Peter has been diagnosed with early osteoarthritis in both knees and has been experiencing acute low back pain.
Peter has been told by his physician to lose weight.
Upon examination of the lifestyle and health risk questionnaire that Peter completed during his profile appraisal, it was noted that he was classified as moderately at risk. This was decided upon by the two risk factors of obesity and sedentary lifestyle that he demonstrated.
Peter’s fitness appraisal reported a resting heart rate of 80 beats per minute and maximum heart rate of 175 beats per minute. A submaximum VO2 max cycle test indicated his aerobic capacity to be 30ml.kg.min-1.
The initial realistic goal that Peter should strive for is a reduction in body fat to 30%.
Goal Weight
Peter’s Goal weight = 99 kg Exercise Prescription
When developing Peter’s exercise prescription it is important to note his osteoarthritic knees by encouraging him in non-weight bearing exercise.
Peter has a background in cycling and has decided that his focal exercise mode will be cycling in the cardio theatre environment.
This exercise session performed 5 days per week is the main weight loss intervention that Peter will be prescribed.
Peter’s initial level of aerobic fitness is quite low (30 ml.kg.min-1) and as such he should exercise at an intensity within a heart rate range of between 60%- 70% HRR.
Peter’s target heart rate during his exercise session will be:
Target heart rate (lower level) = (intensity fraction) x (HR max- HR rest) + HR rest
Target Heart rate (lower level) = (.60) x (175-80) + 80 Target heart rate (lower level = .60 x 95 + 80
Peter’s target heart rate (lower level) = 137 beats Target heart rate (upper level) = (.70) x (175-80) + 80 Target heart rate (upper level) = .70 x 95 + 80 Peter’s target heart rate (upper level) = 147
Peter’s target heart rate range = 137 – 147 beats per minute
For Peter to maintain his heart rate between 137–147 beats per minute, he must pedal on the bike at 90 watts or 540 kg.m.min-1 (one watt is approximately equal to 6 kg.m.min-1).
What is Peter’s oxygen consumption?
We can determine this by using the following calculation:
- VO2 = 7 + 1.8 x (work rate in kg.m.min-1) ÷ (divided) by (body mass)
- VO2 = 7 + 1.8 x (540 kg.m.min-1) ÷ (divided) by 110 kg
- VO2 = 7+ 972 ÷ (divided) by 110
- VO2 = 979 ÷ (divided) by 110
- VO2 = 8.9 ml.kg.min-1
This indicates that when Peter cycles on the stationary cycle at a heart rate between 137-147 beats per minute at 90 watts he will consume 8.9 ml.kg.min- 1.
Convert 8.9 ml.kg.min-1 to litres of oxygen per minute
= (8.9 ml.kg.min-1) x (110 kg) = .98 litres of oxygen per minute divided by 1,000
To calculate the number of Kilocalories expended per minute multiply litres per minute by 5 Kilocalories expended (20.9 kJ) = .98 x 5 = 4.9 Kcal per
minute (20.5 kJ)
If Peter exercises on his stationary cycle for 60 minutes per session he will expend (4.9 Kcal per minute x 60 minutes) = 294 Kcal per exercise session (1230 kJ).
Peter currently weighs 110 kg and has a goal weight of 99 kg for a total weight loss of 11 kg.
If Peter exercises 5 days per week for 60 minutes at a heart rate range of 137–147 beats per minute he will expend 294 Kcal per 60 minute session x 5 sessions per week = 1470 Kcal per week (6,154 kJ)
In order for Peter to lose I kg of body weight he would need to expend 7,700 Kcal.
Peter ‘s goal is to lose 11 kilograms or expend 84,700 Kcal (354,638 kJ).
How long will it take Peter to reach his goal body weight?
If Peter expends 1470 Kcal per week it will take him (84,770 Kcals) = 57 weeks to lose 11 kilograms if he maintained his present eating habits.
This tells us that the one hour per day five days per week that Peter is exercising at the gym is not producing the rapid weight loss that we have been told exercise will create. If Peter does not supplement his exercise program with additional daily movement there is a possibility that if all things do not remain equal he could put weight back on.
It is becoming much clearer that weight loss is a long process that requires a behavioural change as well as change in mind set where we are required to move at light to moderate intensity throughout our day at home, at work, during leisure times and while transporting.
We can never underestimate the importance of what we eat and how much we eat!
Simply by adding daily active lifestyle movements Peter could potentially expend another 500 Kcals of energy expenditure per day, which is over 200 Kcals more than the formal exercise session produced.
If Peter (classified as obese) was exposed to a high intensity exercise session before he was prepared for it, he would still only expend less than 500 Kcals per session. He would also then be potentially exposed to joint and muscle injuries, over production of free radicals, inhibition of nitric oxide in the blood vessels and other overuse or overtraining symptoms.
What do you think the answer is?
Never underestimate the value of small steps…
If we replaced some of our sedentary activity time (< 1.5 METS), by light intensity movement (1.6-2.9 METS) there could be potentially an increase in our energy expenditure of one additional Kcal. E.g. standing rather than sitting.
If we continued this for 50% of our 8 hours working day we could be in Kcal deficit of more than 240 Kcals per day.
Accumulated over a 5 days working week the energy deficit could become 1200 Kcals plus weekend activity. This could translate into approximately 1 kilogram of body weight lost per month all other things being equal.
Without any other intervention it is possible to lose in excess of 12 kilograms of body weight per year with very little change in our normal behaviour.
If we employ additional movement during our leisure time, home time and travelling to and from work greater significant changes to our body weight could be made without additional financial cost and time.
Body weight changes are also accompanied by significant physiological changes that can potentially reduce risk factors and create a much healthier disposition than can result from less prolonged sitting.
Light intensity activities performed multiple times throughout the day can contribute significantly to the total energy expenditure. This supports the concept that both prescribed exercise at a moderate to vigorous intensity and multiple bouts of low intensity activity both contribute to significant independent health benefits and increased energy expenditure.
Sadly many people want instant weight loss and are not prepared to change their lifestyle for long-term weight loss. In most cases 90% of people who start on intense intervention weight loss programs without a lifestyle intervention will put that weight back on within 12-18 months.
Do not underestimate the impact that light to moderate physical activity can have on your overall health as well as significant long-term weight loss.
There is always a consequence…..what the wrong type of physical activity can do to your blood vessels..
Cardiovascular disease is amongst the leading causes of death in the developed world, often associated with affluence and economic growth.
One risk factor acutely associated with cardiovascular disease is endothelial dysfunction. The endothelium is the inner lining of blood vessels responsible for the dilation and constriction of the blood vessel, regulation of the nerve supply, promotion of vascular changes, the control of inflammation, and increases in the production of nitric oxide.
The endothelium covers all the internal surfaces of blood vessels, cardiac valves and other internal cavities. Any imbalance in these functions causes a condition called endothelial dysfunction. This imbalance can be caused by the unavailability of nitric oxide (NO), an increase in free radical production and an increase in endothelial activity.
Risk factors associated with endothelial dysfunction include smoking, obesity, diabetes, hypertension, high cholesterol levels and sedentary behaviour.
Aerobic exercise produces positive changes in nitric oxide (NO) production in the lining of the artery, increase in vascular endothelial growth factor and an increase in the antioxidant defence system.
If the formation of nitric oxide is low in a number of different blood vessels there is a potential reduction in blood flow to the inner lining and the formation of a coagulation or eventually a clot, damaging the arterial wall and predisposing the body to the onset of cardiovascular disease. On the other hand an excess of nitric oxide can result from dilation of vessels and the promotion of shock due to the redistribution of blood flow.
Any damage to the endothelial wall has been reported as the starting point for atherosclerosis (narrowing and hardening of the arteries) and/or cardiovascular disease.
In ageing endothelial dysfunction is regarded as the starting point to cardiovascular damage. Damage to the endothelial changes the vessels dilation responses, anti-clotting mechanisms and produces ongoing adverse structural changes.
Regular moderate physical activity can enhance blood vessel structure and improve its function by an increase in blood flow. These long-term responses occur to a greater degree in slow twitch motor units that are more sensitive to moderate intensity physical activity performed for longer time periods either continuously or discontinuously.
One of the damaging changes to the endothelium is the insufficient supply of nitric oxide, which is caused by oxidative stress (uncontrolled free radical production), inflammation of the lining of the blood vessel, erosion of the cells and the constriction of the blood vessel.
These free radicals cause the deactivation of the endothelial receptors responsible for the production of nitric oxide, which stops the endothelial cells from dilating potentially causing a build up of plaque and a narrowing of the blood vessels.
While the benefits of physical activity such as positive changes in blood pressure, blood lipid profiles and glucose metabolism are widely known to improve endothelial (artery wall) performance, the exercise intensity to improve these components is still open to debate.
As a general rule moderate intensity physical activity on a frequent basis improves health by improving the antioxidant defence mechanisms in both healthy individuals and those diagnosed with hypertension.
In more vigorous or high intensity exercise, there is a greater production of uncontrolled free radicals that can have a potential negative effect on both skeletal and cardiac muscle tissue. It must be remembered that the intensity whether it be fitness centre based or lifestyle based is relative to the fitness of the individual as well as their health status. Unfit people can improve their VO2 max with what a fit individual would regard as moderate intensity yet intense for the unfit.
There seems little doubt that improvements in maximum aerobic capacity are dependent upon vigorous high intensity activity indicating that aerobic fitness improvements are intensity based.
Responses such as cardiac muscle hypertrophy and calcium handling are more sensitive to vigorous exercise generally of a discontinuous or interval raining nature.
Conversely moderate intensity appears to produce more significant changes in endothelial function.
In any type of aerobic activity it is important to improve the muscle’s blood flow and arterial conductance in order to improve general physical performance. However, endothelial changes appear to reach their maximum effect at moderate intensity mainly due to increased production of nitric oxide at these levels.
One study reported that high intensity occupations over a long time period in males aged between 42-60 years of age was associated with accelerated progression of carotid atherosclerosis (narrowing and hardening of arteries in the neck) indicating an impaired functioning of the blood vessel endothelium at higher levels of intensity.
The position at the moment suggests that high intensity exercise that is beyond the capability of the individual can result in a turning off the production of nitric oxide in the walls of the artery potentially initiating adverse changes leading to atherosclerosis or hardening of the arteries.
Physical activity must be progressive in nature. We should start at the lower to moderate intensity levels building to the more intensity training methods.
Some unfit, overweight, older and or younger clients can be placed at risk without a progression to high intensity physical activity.
Remember if you are training clients you have a “duty of care” to ensure a safe exercise environment.
