
Article by Gill Cummings-Bell BA (Hon’s) M.Sc. PGCE. MBA
Why Therapy Exercise?
The key area for any therapy exercise is to be able to identify how exercise relates to the condition presented. Exercise therapists must have the skill to observe technique closely and be able to understand dysfunctional movement patterns caused by poor posture, musculo-skeletal injury or instability. They must also be able to analyse the exercise rehabilitation needed and be consistent in observation of outcomes. It is essential to understand the implications and contra-indications that each dysfunction or injury has regarding exercise. In order to understand what is needed and to be effective as an exercise professional in this specific field, the basic pathology of the dysfunction or injury is required as well as where exercise fits as a benefit and a rehabilitation.
There are many forms of musculo-skeletal injury or problems. For this article we will take a brief look at injury caused through exercise in general and postural dysfunction.
Injury Overview
Exercise injuries can be classified as either acute or overuse injuries. Over the past few decades more and more overuse type injuries have been reported. This changing trend is the result of the increase training demands clients are placing on their bodies, in addition to the increasing popularity of endurance events such as triathlons,marathons and enduro-typeevents.
Acute injuries can result from either intrinsic (indirect) factors or extrinsic (direct) factors. Intrinsic factors include twisting an ankle or falling onto an outstretched hand. Extrinsic factors include direct contact with another player or equipment.
Acute injuries are obvious and painful to a client. They are usually the result of a collision, fall or twisting injury and pain is felt immediately. The most common acute exercising injuries are ligament sprains and musclestrains.
Overuse injuries from repeated micro trauma are often less obvious to the client due to a gradual onset of pain. These injuries are usually the result of poor biomechanics, dysfunctional movement patterns, poor posture, an inappropriate increase in training, faulty technique, muscle weakness or in flexibility or insufficient recovery.
The Pain Threshold
Clients/patients tend not to seek help for an injury until a niggle overtime has reached a pain threshold. See fig.1.
Fig. 1 Pain over time threshold
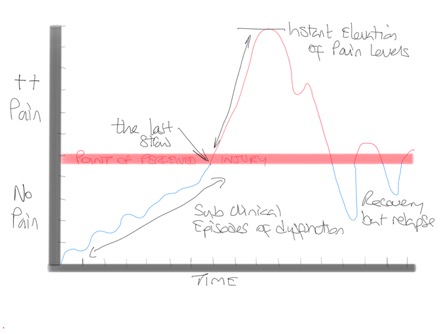
In overuse injuries one or more of these factors can lead to local tissue damage and degeneration. If tissue damage is not recognised, and given no time to heal, it can progress to stress fractures, ligament strains, synovitis, compartment syndrome, with tendinitis being the most common overuse injury.
Primary injuries are caused by a directtrauma to a site. For example, an individual twisting to turnaround or falling the wrong way causing tearing of the medial collateral ligament can be a primary injury. A secondary injury can manifest itself sometime after the injury occurred, if a client suffers a primary injury and then compensates for this injury by altering their normal movement.
The mechanism for suffering an injury can be due to direct impact, excessive overload, general overuse, structural vulnerability, inflexibility, muscle imbalance or rapid growth, a dysfunctional movement pattern, or poor posture and form.
The body’s response to both acute (macro-trauma) and overuse injuries (micro trauma) is known as the inflammatory response. Inflammation is the body’s internal defence mechanism to overcome stress and return the body to its normal state of homeostasis (body in balance). Macro injuries can be caused by repeated trauma of the micro injuries. For example, in many cases stress fractures of the tibia can initially manifest itself in acute shin soreness, with repeated loading eventually leading to stress fractures.
Acute injuries tend to occur more in the younger age groups while with advancing years’ chronic injuries are more prevalent. This is partly due to the loss of strength and density of tissues that occurs with age. The decrease in function is often a result of the training and functional age of the client. There are many 50 years old active males and females that may have greater muscular strength and bone density than much younger adults.
Females tend to suffer more bone related injuries due to their propensity for osteopenia, leading to osteoporosis. This is especially true of post-menopausal females.
There is a strong correlation between the training age and degree of overall fitness and the reduced potential for sustaining an injury. If an injury does occur there is every likelihood that the client with the longer training age will recover at a much faster rate. If you are fit and strong and take part in regular physical activity or exercise you will recover more quickly and are less likely to suffer injuries.
Other factors that impact on sustaining and rehabilitating an injury are sedentary lifestyle, nutrition, fatigue, skill level, previous injury, posture, movement and the environment and in some cases equipment or facilities.
Inflammation
The inflammatory response is the generalized response that occurs at an injury site because of acute or chronic trauma.
Inflammation is characterised by redness, pain, and loss of normal function, heat and swelling. These signs are often referred to as the four cardinal signs and correspond to the various stages of cellular response to trauma. The increased swelling can cause pain due to the increase in pressure and bleeding into a joint as well as on nerve endings.
Initially the response to an injury is a decrease in blood flow known as the coagulation phase. This is rapidly followed by an increase in blood flow to the affected area. Vasodilation (increase of blood vessel diameter) of the surrounding veins, arteries and capillaries enables the increased flow of blood. Increased blood flow not only takes defensive substances (white blood cells and clot-forming substances) to the area but enables a greater removal of toxic products and dead cells from the area and brings with its fibrinogen and plasma proteins.
The inflammation is controlled by chemical mediators such a histamine, serotonin, bradykinin, prostaglandins, leukotrienes and plasmin. Phagocytes accompany the chemical mediators to clean and clear any debris.
The heat that can be felt over a site of injury is the result of an increased blood flow and an increase in the metabolic rate of the surrounding tissue as it begins to repair.
Pain at the site of injury can be the result of several mechanisms. Pain can be a result of mechanical or chemical stimulation. Stimuli for pain includes excessive stretch, prolonged muscular contraction, muscle spasm, reduced blood flow to an area or the presence of chemicals released from the damaged area (prostaglandins, histamine).
There are three main structures that cause musculoskeletal pain: joints (including ligaments), muscles (including tendons and fascia) and nerves. Pain felt by a client may arise from one or all of these structures.
Joint Pain
Pain sensitive nerve endings are found throughout alljoints in the body. The nerve endingswithin the joint may be stimulated as a result of chemical irritation or mechanically as a result of over-stretching of the joint, impact or a breakdown of structures.
Muscle Pain
Muscle pain is often described as dull, cramping and aching. It can be the result of acute injury or in association with other injured structures. Often damage to a joint can result in a protective muscle spasm. If pain and inflammation of the joint persists the muscle spasm will eventually lead to both mechanical and chemical irritation of the surrounding nerve endings.
Neural Pain
Pain arising from injuries to neural structures (structures of the nervous system) is often described as shooting and sharp. Neural structures like muscles and joints have nerve endings that can be irritated chemically or mechanically. Increased neural tension as a result of trauma or injury will lead to pain. Pain is often associated with altered or poor mechanics. The restoration of normal mechanics and full range of movement is critical for pain-free movement.
Referred Pain
Pain is usually perceived as coming from the site of injury, e.g. pain from an ankle sprain will be felt in and around the ankle joint. However, pain can originate from a site away from where the client perceives the pain, this is known as referred pain. A typical example is of a client, who perceives pain in the hamstrings, however, athorough clinical history and examination reveals no injury to the hamstring, and little or no loss of strength and flexibility. The client describesa dull and deep pain that is difficult to localise. This type of pain is likelyto be referred from pain sensitive structures of the lower back.
Repair of injured tissue takes places over three stages: the acute, sub-acute and chronic stages of healing. The acute stage of healing is characterised by an inflammatory response where vascular changes, clot formation and cleaning up of the inflamed site begin. The clinical signs of this phase of healing are the four cardinal signs of heat, redness, pain and swelling. The aim of treatmentat this stage of healing is to reduce inflammation using therapeutic modalities with gentle mobilisation or with complete immobilization.
When pain is not what it seems
On occasions a client who presents with what appears to be an exercise related injury, may in fact be something moresinister. Only after a thorough history, clinical examination andappropriate investigations can a correct diagnosis be made. Often the clinician realises that the history and the physical examination do not fit theusual clinical picture. For example, the client may complain of mid-thoracic spine pain, worse with exercise, but with no relief at rest. The client might also complain of night pain, which wakes them during sleep, general tiredness, loss of appetite and weight loss. If a client reports pain in any part of the body, in addition to any of the above-mentioned factors a thorough examination is crucial to determine the exact cause of pain.
Tissue Types
Tissue consists of four basic types: epithelial, nervous, muscle and connective. The epithelial tissue functions to absorb, secrete, transport, cover or protect tissues or organs. Epithelial tissue is constantly being replaced and regenerated due to basic wear and tear. Epithelial tissue is classified according to the number of cells that it comprises and the structure that they form. A simple epithelial tissue consists of a single layer of cells, while stratified epithelial consists of two or more layers of cells. The formation of layers of cells can be classified as flat (squamous), cuboidal (cube shaped) or columnar (column shaped).
Tissue Repair
During the sub-acute stage of healing (3-7days after injury) the removal ofchemical irritants that havea pain producing effect is achieved. Tissuerepair commences during the inflammatory stages; however, it can only be completed after all harmful substances have been neutralised or removed from the site of injury. There is also agrowth of new capillaries into the area, which improves oxygen and nutrient flow to the newly forming tissue. Collagen, a strong dense connective tissue is laid down to add tensile strength to the healing tissue along with granulation tissue that acts as a strong framework for new cells to begin to grow. Theprimary aim of treatment during this phase is to prevent orminimise muscle shortening. This is achieved by gentle passive or active range of movement exercises that slowly progress to increase both range and speed of movement.
The final stage of tissue repair is known as the chronic stage. This involves the maturation and remodelling of tissue. Collagenous tissue continues to mature and remodel as part of the healing process for 6 to 12 months. For the proper alignment of collagen fibres and remodelling of scar tissue it is vital to place continuous levels of mechanical stress upon the healing tissues. The aim of this phase of healing is to restore function. This is achieved through progressive stretching, strengthening and functional exercises.
Bone Injuries
The structure of bone allows a strong core to be imbedded into a flexible outer surface. This property allows bone to be particularly strong and stiff andat the same time very flexible. When abone is deformed, or loaded, its initial response is to bend and then recover to its original shape. The change in the shape of the bone is not permanent. However, when the bone is loaded to its optimal point, the outermost fibres begin to change shape indicating its elastic limit. If load is continually added the bone undergoes a second deformation that remains even when the bone returns back to its original position and injury can result.
In children, bone growth occurs at the epiphyseal growth plates. These growth plates are located between the shaft and the end of the long bones. The growth plate consists of three zones (growth, maturation, transformation) each consisting of chondrocytes that are responsible for the growth of the bone. At maturity, these epiphyseal growth plates close and no further growth can occur. At the site of the attachments of muscles on the bone are small growth plates called apophyses that are responsible for the shape of the bone. Mechanical stresses placed on bone within its limits can have a positive effect on bone growth. Other factors such asthyroxine, oestrogen, growth hormone and testosterone can also have an influence of bone growth.
It has been reported that up to 15% of all fractures in children occur at or involve the epiphyseal growth plate. Females tend to be more prone to epiphyseal injuries between 9-12 years, while males are more prone from 12-15 years. If an injury involves the growth plate, there is always the possibility of premature growth plate closure resulting in growth retardation.
The most common bone injury is a fracture. Fractures can be a result of a direct blow or implement or indirectly as a result of a twisting injury or from overuse as seen in a stress fracture of the lower leg. Direct force on a bone can cause different types of fractures. Small repetitive forces over an extended period of time can cause transverse fractures that extend directly across the bone. Crushing forces cause multiple fractures to the bone usually along different lines. High velocity penetrating forces create a crushing injury usually to the centre of the bone.
Indirect forces can create traction fractures such an avulsion fracture (ligament pulls off its bony attachment). An angulation force can cause the bone to snap at its middle. Rotational forces can cause spiral fractures. Vertical compression causes oblique fractures. If a bone is repetitively loaded beyond its level of strain a stress fracture or micro fracture of thebonewillresult.Therearecurrentlytwotheoriesonhowstressfracturesoccur. The fatigue theory supports the idea that muscle fatigue leads to an increased stress on the bones.
The overload theory suggests that with each muscle contraction and then relaxation the bone is flexed backwards and forwards. This constant movement of the bone leads to tiny cracks appearing and the bone becomingweak.
Thinner bones such as thetibia are at a greater risk ofdeveloping stress fractures. Indirectfractures can occur when connective tissue is stressed andas a result pulls on its bony attachment. As the force of the connective tissue is greater than its attachment to the bone an avulsion fracture can occur. This is when the bony attachment is pulled off the parent bone. This most often occurs with ligaments or tendons.
Some types of bone are more susceptible to fractures than others. Trabecular or cancellous bone found in the shaft of the bone, because of its latticework structure appears to be more prone to fractures. While the denser cortical bone found at the end of bones is more fracture resistant.
Another bone condition is osteoporosis, which refers to a breakdown of bone, particularly devastating at weight bearing joints. As ageing occurs there is a progressive bone loss leading to osteoporosis caused by diet, activity patterns, hormonal changes and calcium deficiencies.
Postural Dysfunction and Corrective Exercise: What are they?
Good posture and how stable the body is in postural positions is the product of the force generated by four myofascial/muscle slings that are located diagonally throughout the body. Often referred to as the sling systems.
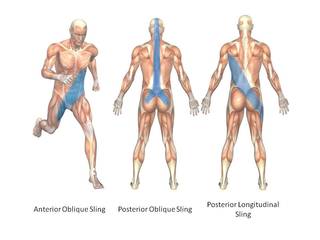 The four myofascial/muscle slings are the anterior oblique sling, the posterior oblique sling, the deep longitudinal sling and the lateral sling.
The four myofascial/muscle slings are the anterior oblique sling, the posterior oblique sling, the deep longitudinal sling and the lateral sling.
The posterior oblique slingconsists of the latissimus dorsi that extends diagonally through the thoracolumbar fascia and blends with fibres of the opposite gluteus maximus. The superficial fibres of the gluteus maximus then blend with the superficial fibres of the TFL and ITB on the side. The function of the posterior oblique sling is to provide a counter rotation force between the upper body and the lower body that produces tension in the thoracolumbar fascia stabilising the sacroiliac joint and the pelvis.
During the push off phase of walking, the hip joint extends to push the ground away from the body. As hip extension is initiated by the contraction of the gluteus maximus, the opposite latissimus dorsi contracts to bring the opposite shoulder joint into extension creating a counter rotation of the upper and lower body and increased pressure on the thoracolumbar fascia.
The anterior oblique slingconsists of the external oblique, internal oblique and the transverse abdominis through the rectus sheath blending with the adductor muscles on the opposite side (contralateral) and their fascial sheaths. The purpose of the anterior oblique sling is to stabilize the trunk and lower body during movement. As the lead leg contacts the ground in walking, the lead leg adductors work with the internal oblique on the same side and the external oblique on the opposite side stabilising the trunk on top of the lead leg. The activation of the anterior oblique sling becomes more dominant when the client progresses from walking to running.
The deep longitudinal slingconsists of the multifidus, which attaches to the deep thoracolumbar fascia while blending with the Sacro-tuberous ligament and the biceps femoris extending to the peroneus longus. The deep longitudinal sling is an important shock absorption system for the body in walking and running. When the lead foot contacts the ground the peroneus longus works with the tibialis anterior to stabilize the foot and the ankle. As this force is dispersed up the leg it is taken up by the biceps femoris, who while attempting to control hip flexion and knee extension transfers it to the sacro-tuberous ligament. At this point energy is captured in the thoracolumbar fascia to be used in the propulsive phase.
The lateral slingconsists of the gluteus medius, gluteus minimus and the same side adductor muscles (ipsilateral) and the opposite side quadratus lumborum (QL). The purpose of the lateral sling is to provide stability in frontal plane during any lower body movement performed in the sagittal plane e.g. walking and running. At heel strike the hips maintain the weight of the body by the gluteus medius and gluteus minimus contracting to keep the ilium and the femur together. At the same time the quadratus lumborum on the opposite side assists in elevating the ilium.
In a step-up action, the support leg will be stabilized by the same side gluteus medius and adductor longus, adductor brevis and adductor longus. To bring the lead leg up to the step, the opposite quadratus lumborum will elevate the same hip to allow the foot to contact the step.
How the Slings Influence Postural Dysfunction
The influence of gravity combined with the movements that are now required for clients to perform their daily activities has created a body that presents with predictable patterns of muscle imbalances that can lead to dysfunctions in the muscle slings. Muscle imbalances are caused by a variety of factors. Postural dysfunctions can alter a client’s movement patterns and cause compensatory mechanisms to take place in other parts of the body. Movements that are in the same movement pattern can cause a change in the relation-ship between agonists and antagonists. i.e. Poor trunk strength can provide a weak platform from which other limb movement patterns can be initiated causing an abnormal development of agonists and antagonists.
There are many reasons postural dysfunction can occur as well as distortion in the muscle slings although we are increasingly seeing the dysfunction caused by poor movement patters at a young age due to sedentary lifestyle patters. Ageing can also cause significant bone changes, joint changes and muscle changes leading to dysfunctional postures. Injury or immobilization of a limb can cause compensatory movements at joints, while fatigue without adequate recovery can also cause changes in movement. All lead can lead to postural dysfunction.
Clients who spend many hours of the day in prolonged postures i.e. sitting at computers and at a desk, driving for long periods or sitting in meetings result in a significant shortening and lengthening of associated muscles, e.g. sitting postures. When specific muscles become habitually shorter their length tension-relationship becomes compromised. This in turn decreases their force production and alters their relationship with their antagonist muscles producing muscle imbalances caused by a neural insufficiency. Muscle can become tight and short or weak and long.
The three postural syndromes that can be caused by tight/short and or weak/long muscles are the upper cross syndrome, the lower cross syndromeand the pronation distortion syndrome.
The uppercross syndromeincludes tight upper trapezius, levator scapulae, pectoralis minor and pectoralis major and weak lower trapezius, rhomboids and deep flexors of the neck leading to upper cervical lordosis giving the impression of a sunken neck. This is typically seen in clients with round shoulders and forward head. Some of the symptoms of upper cross syndrome are daily headaches, stiff neck, muscle spasms in the lower back and upper trapezius and shoulder impingement.
The lower cross syndromeis recognised by a forward tilt of the pelvic girdle and hyper-extension of the lumbar spine. This specific syndrome is caused by a weak gluteus maximus, gluteus minimus and gluteus medius, weak abdominals, tight lumbar spinal extensors, tight iliopsoas and tight TFL. The specific muscles that tend to be tight and short and need stretching include the iliopsoas, erector spinae (lumbar section), rectus femoris, TFL, quadratus lumborum, adductor longus, adductor magnus, adductor brevis and the hamstrings. The muscles that are weak and in need of strengthening include the gluteus maximus, gluteus medius and gluteus minimus and the abdominal muscles.
The pronation distortion syndromeis observed in clients that present with knock knees and pronated ankles and/or flat feet and tibial torsion. The specific muscles that tend to be short and tight include the gastrocnemius, soleus, ITB, hamstrings, adductors and the iliopsoas. Those muscles that tend to be long and weak are the tibialis anterior, flexor digitorum longus, flexor hallucis longus, tibialis posterior, vastus medialis, gluteus medius and gluteus maximus.
Other problems may also occur through lifestyle patterns that restrict movement such as synergistic dominance. When a tightening or shortening develops in a strong muscle it causes a reciprocal inhibition
in its antagonist muscles. The resulting inhibition of the antagonist muscles leads to a decrease in neural activation of the opposing muscles contributing to further muscle imbalances. As these agonist muscles become shorter and stronger and their antagonists becomes weaker (loss of strength), other agonist muscles within the muscle group become dominant, causing altered movement patterns. This has been referred to as synergistic dominance. For example, in the case where a client sits for long periods the hip flexors become short and tight which causes a shutting down or inhibition of the gluteal muscles (reciprocal inhibition and neural insufficiency). Since the gluteal muscles are no longer working correctly the body will begin to recruit the hamstrings (synergistic dominance) and the low back muscles to assist the gluteal muscles in hip joint extension, leading to postural and movement pattern dysfunction.
Myo-fascial Therapy Exercise Objective
In a therapy exercise program, the short/tight muscles are released by stretching techniques that include static stretching, dynamic stretching, PNF stretching and CRAC.
The fascia is released through myofascial release techniques and trigger point therapy. Self-myofascial release (SMR) techniques (foam rollers, tennis balls) activate the nervous system sensory receptors in releasing muscle tension through autogenic inhibition. This reflex activates the Golgi-tendon organs forcing the muscle’s stretch reflex to be inhibited, releasing muscle tension. It has the added benefit of releasing restrictive fascial tissue that surrounds the muscle component.
i.e. in the case described above of synergistic dominance, initially the corrective exercise specialist would prescribe stretching exercises for the iliopsoas, rather than strengthening exercises for the gluteal muscles. By increasing the length of the hip flexors, it is possible to improve the activation of the gluteal muscles followed by a more formal strengthening program for these muscles. A full body integrated strength program can then be prescribed to strengthen the weak or atrophied muscles by recruiting all the functional muscles in the body in large muscle movement patterns. Compound or isolated agonist movement patterns can also be prescribed to recruit specific muscle groups or specific muscles that require strengthening.
To become a corrective exercise specialist, you require a deep knowledge of anatomy & physiology, biomechanics and corrective exercise techniques. A worthwhile area of work and one that can increase your reputation and make you stand out from the crowd.
Injury Therapy Exercise Objective
The aim of rehabilitation is to reverse the effects of immobilization. Although immobilization is a necessary part of the healing phase of any injury, prolonged immobilization will lead to significant loss of muscle strength and endurance, flexibility, proprioception and co-ordination. Return to exercise should only take place when the client has regained full range of movement, normal muscle strength, power, endurance and exercise specific skills.
It is important to remember that just because an injury has healed it does not mean that the client is ready to return to exercise. The client must not return to exercise if it will placea stress on the injured tissue causing pain, swelling, inflammation or restriction of movement.
The basic goals of a rehabilitation program include: regaining muscle strength, power and endurance,regainingjointrangeofmovement,regainingjointstability,regainingproprioception of the injured joint and limb, and regaining exercise specific skills. It is also necessary to address any postural, anatomical or biomechanical dysfunctions that may have contributed to the initial injury
Regaining Muscle Strength, Power and Endurance
A common error when rehabilitating weak muscles is to do too much too soon. When regaining strength of an injured muscle is it necessary to start with a low resistance and high repetition program, which is then progressed to a higher resistance, low repetition program. As the strength of muscle groups improve, the client can then add eccentric contractions and more functional exercises to the program.
To regain muscle strength, it is possible to use water resistance, elastic resistance bands, manual resistance, body weight resistance, cable pulley resistance, machine weight resistance, barbell resistance, dumbbell resistance etc. depending on the level of the client’s rehabilitation.
Muscle endurance is the muscle’s ability to continually contract. Initially in exercise rehabilitation it is necessary to regain muscle endurance through isometric contractions. This is seen in many bridging and bracing exercises prescribed for spinal rehabilitation. This procedure can then be followed by isotonic exercises with different forms of resistance.
Aerobic endurance can be achieved or maintained through low resistance, high repetition exercises, such as swimming, cycling, circuit training, cardiovascular machines such as steppers, stair climbers, treadmills, elliptical machines, rowers etc.
Regaining Joint Range of Movement
Following an injury, joint range of movement is often significantly reduced. Swelling, inflammation and pain will all result in a stiff and painful joint. Early mobilization of the joint has a positive effect on ligaments, tendons and muscles and helps prevent adhesions and scarring within and around the joint.
Many techniques can be used both to avoid joint stiffness – passive mobilization, passive stretching, active exercises and active assisted exercises, myofascial release techniques.
To ensure muscles remain flexible it is necessary to include myofascial release techniques with mobility and stretching exercises as part of the rehabilitation program. In correcting postural distortions or dysfunctional movement patterns prescribing self-administered myofascial release techniques with mobility and stretching exercises is the first step in treatment.
Proprioception
Proprioception can be defined as a sense of joint position‚ or kinesthetic awareness or more simply an ability to judge where a body part is in space. Any joint injury can lead to direct or indirect disruption of proprioceptive awareness. Mechanoreceptors within the joint provide feedback sensory information to the brain describing joint position, motion and pressure. Destruction of these receptors can lead to a proprioceptive loss and an increased chance of re-injury.
Proprioceptive exercises are not stressfulon healing tissue and can begin very early in the rehabilitation program. It is important to progress the client through a series of proprioceptive exercise.For example, in lower limb injuriesthe client may start with low level co-ordination exercises, and supportedone-legged balancing exercises progressing to, non-supportive, then more unstable surface such as a wobble board, mini-tramp, bosu ball, fit ball and freeform boards etc. Once these basic exercises have been practiced more challenging proprioceptive exercises can be used such as skipping drills, sideways and backwards running, cutting sharply through markers.
Regaining Joint Stability
Regaining joint stability focuses on achieving a balance between agonist and antagonist muscle groups. Stabilization is a vital component of low back, shoulder, groin and pelvic rehabilitation. Dynamic lumbar stabilization is now well researched and considered an integral part of every lower back pain rehabilitation program. Lumbar stabilization involves the progressive retraining of the normal movement patterns of the muscles of the trunk, abdominals and back. Shoulder stabilization focuses on regaining co-contraction of the stabilizers and movers of the shoulder assisting in regaining smooth glenohumeral rhythm.
Regaining Exercise Specific Skills
Rehabilitation is not complete until the client can perform functional exercise specific skills at a maximal level without pain or loss of function. In addition to placing maximal stress on the newly repaired tissue, these skills will fine tune proprioceptive and neuromuscular pathways that are specific to the client’s functional exercise needs.
As you can see working in Therapy Exercise is a challenging area involving deepening your knowledge and understanding of anatomy & physiology, biomechanics, medical conditions and exercise micro control just to name a few areas. It is also a very rewarding area of work where you can have the most impact on your client’s life and well-being. You can really help clients regain high level function and therefore a great quality of life.
If you are interested in this area of work why not choose your preferred discipline and book your place on our Exercise Therapy Module or our advanced Level 4 Pilates Matwork or Level 4 Personal Training or Level 4 Back Pain or our Sports Massage Diploma.
Use your graduate voucher and book your place today.
