Good posture and how stable the body is, in varied postural positions is the product of the force generated by four myofascial/muscle slings that are located diagonally throughout the body. Often referred to as the sling systems.
The four myofascial/muscle slings are the anterior oblique sling, the posterior oblique sling, the deep longitudinal sling and the lateral sling.
The posterior oblique sling consists of the latissimus dorsi that extends diagonally through the thoracolumbar fascia and blends with fibres of the opposite gluteus maximus. The superficial fibres of the gluteus maximus then blend with the superficial fibres of the TFL and ITB on the side. The function of the posterior oblique sling is to provide a counter rotation force between the upper body and the lower body that produces tension in the thoracolumbar fascia stabilising the sacroiliac joint and the pelvis.
During the push off phase of walking, the hip joint extends to push the ground away from the body. As hip extension is initiated by the contraction of the gluteus maximus, the opposite latissimus dorsi contracts to bring the opposite shoulder joint into extension creating a counter rotation of the upper and lower body and increased pressure on the thoracolumbar fascia.
 The anterior oblique sling consists of the external oblique, internal oblique and the transverse abdominis through the rectus sheath blending with the adductor muscles on the opposite side (contralateral) and their fascial sheaths. The purpose of the anterior oblique sling is to stabilize the trunk and lower body during movement. As the lead leg contacts the ground in walking, the lead leg adductors work with the internal oblique on the same side and the external oblique on the opposite side stabilising the trunk on top of the lead leg. The activation of the anterior oblique sling becomes more dominant when the client progresses from walking to running.
The anterior oblique sling consists of the external oblique, internal oblique and the transverse abdominis through the rectus sheath blending with the adductor muscles on the opposite side (contralateral) and their fascial sheaths. The purpose of the anterior oblique sling is to stabilize the trunk and lower body during movement. As the lead leg contacts the ground in walking, the lead leg adductors work with the internal oblique on the same side and the external oblique on the opposite side stabilising the trunk on top of the lead leg. The activation of the anterior oblique sling becomes more dominant when the client progresses from walking to running.
The deep longitudinal sling consists of the multifidus, which attaches to the deep thoracolumbar fascia while blending with the sacro-tuberous ligament and the biceps femoris extending to the peroneus longus. The deep longitudinal sling is an important shock absorption system for the body in walking and running. When the lead foot contacts the ground the peroneus longus works with the tibialis anterior to stabilize the foot and the ankle. As this force is dispersed up the leg it is taken up by the biceps femoris, who while attempting to control hip flexion and knee extension transfers it to the sacrotuberous ligament. At this point energy is captured in the thoracolumbar fascia to be used in the propulsive phase.
The lateral sling consists of the gluteus medius, gluteus minimus and the same side adductor muscles (ipsolateral) and the opposite side quadratus lumborum (QL). The purpose of the lateral sling is to provide stability in frontal plane during any lower body movement performed in the sagittal plane e.g. walking and running. At heel strike the hips maintain the weight of the body by the gluteus medius and gluteus minimus contracting to keep the ilium and the femur together. At the same time the quadratus lumborum on the opposite side assists in elevating the ilium.
In a step-up action, the support leg will be stabilized by the same side gluteus medius and adductor longus, adductor brevis and adductor longus. To bring the lead leg up to the step, the opposite quadratus lumborum will elevate the same hip to allow the foot to make contact with the step.
How the Slings Influence Postural Dysfunction
The influence of gravity combined with the movements that are now required for clients to perform their daily activities has created a body that presents with predictable patterns of muscle imbalances that can lead to dysfunctions in the muscle slings. Muscle imbalances are caused by a variety of factors. Postural dysfunctions can alter a client’s movement patterns and cause compensatory mechanisms to take place in other parts of the body. Movements that are in the same movement pattern can cause a change in the relationship between agonists and antagonists. i.e. Poor trunk strength can provide a weak platform from which other limb movement patterns can be initiated causing an abnormal development of agonists and antagonists.
There are many reasons postural dysfunction can occur as well as distortion in the muscle slings although we are increasingly seeing the dysfunction caused by poor movement patters at a young age due to sedentary lifestyle patters. Ageing can also cause significant bone changes, joint changes and muscle changes leading to dysfunctional postures. Injury or immobilization of a limb can cause compensatory movements at joints, while fatigue without adequate recovery can also cause changes in movement. All lead can lead to postural dysfunction.
Clients who spend many hours of the day in prolonged postures i.e. sitting at computers and at a desk, driving for long periods or sitting in meetings result in a significant shortening and lengthening of associated muscles, e.g. sitting postures. When specific muscles become habitually shorter their length tension-relationship becomes compromised. This in turn decreases their force production and alters their relationship with their antagonist muscles producing muscle imbalances caused by a neural insufficiency. Muscle can become tight and short or weak and long.
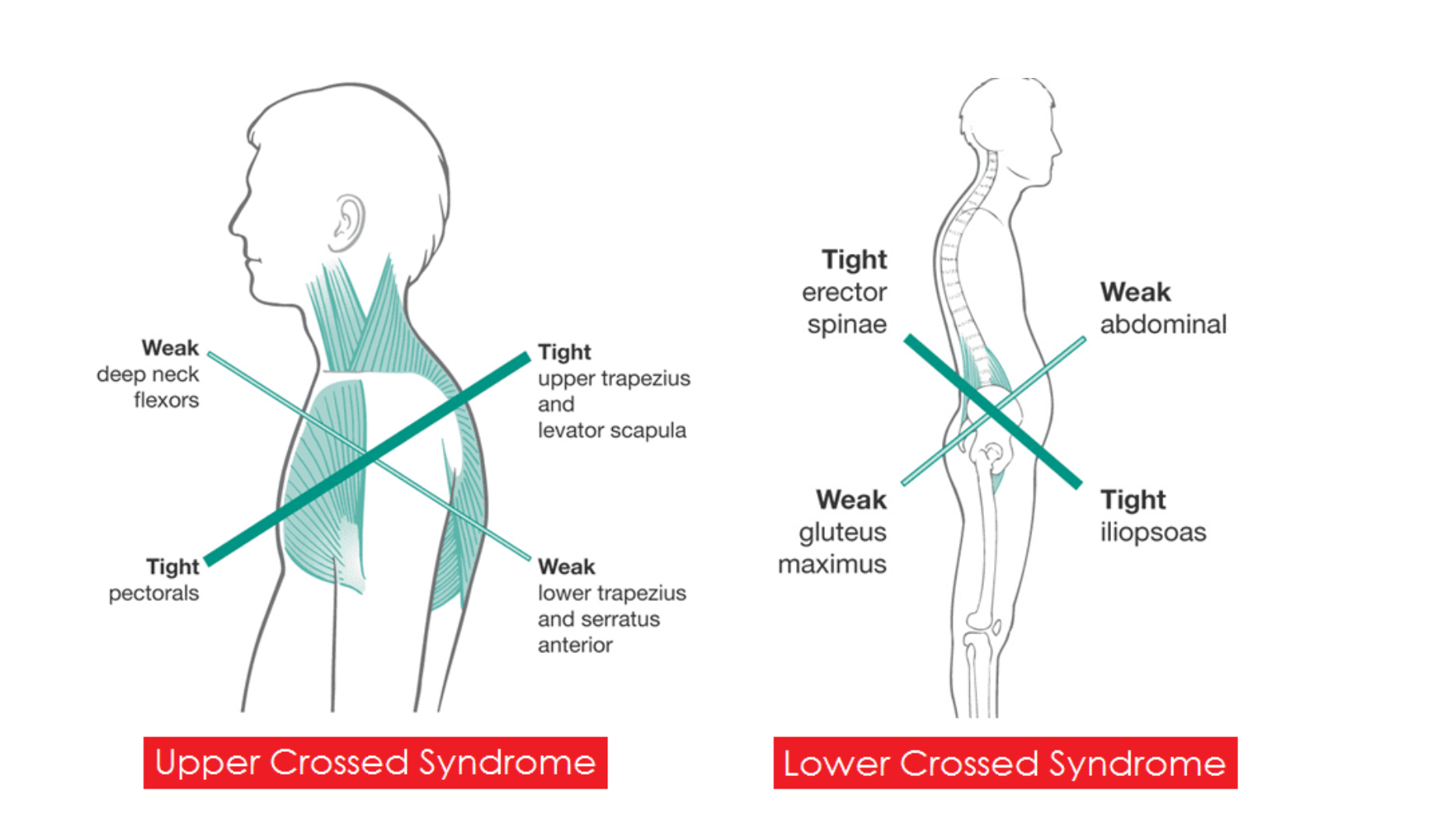
The three postural syndromes that can be caused by tight/short and or weak/long muscles are the upper cross syndrome, the lower cross syndrome and the pronation distortion syndrome.
The upper cross syndrome includes tight upper trapezius, levator scapulae, pectoralis minor and pectoralis major and weak lower trapezius, rhomboids and deep flexors of the neck leading to upper cervical lordosis giving the impression of a sunken neck. This is typically seen in clients with round shoulders and forward head. Some of the symptoms of upper cross syndrome are daily headaches, stiff neck, muscle spasms in the lower back and upper trapezius and shoulder impingement.
The lower cross syndrome is recognised by a forward tilt of the pelvic girdle and hyper-extension of the lumbar spine. This specific syndrome is caused by a weak gluteus maximus, gluteus minimus and gluteus medius, weak abdominals, tight lumbar spinal extensors, tight iliopsoas and tight TFL. The specific muscles that tend to be tight and short and are in need of stretching include the iliopsoas, erector spinae (lumbar section), rectus femoris, TFL, quadratus lumborum, adductor longus, adductor magnus, adductor brevis and the hamstrings. The muscles that are weak and in need of strengthening include the gluteus maximus, gluteus medius and gluteus minimus and the abdominal muscles.
The pronation distortion syndrome is observed in clients that present with knock knees and pronated ankles and/or flat feet and tibial torsion. The specific muscles that tend to be short and tight include the gastrocnemius, soleus, ITB, hamstrings, adductors and the iliopsoas. Those muscles that tend to be long and weak are the tibialis anterior, flexor digitorum longus, flexor hallucis longus, tibialis posterior, vastus medialis, gluteus medius and gluteus maximus.
Other problems may also occur through lifestyle patterns that restrict movement such as synergistic dominance. When a tightening or shortening develops in a strong muscle it causes a reciprocal inhibition in its antagonist muscles. The resulting inhibition of the antagonist muscles leads to a decrease in neural activation of the opposing muscles contributing to further muscle imbalances. As these agonist muscles become shorter and stronger and their antagonists becomes weaker (loss of strength), other agonist muscles within the muscle group become dominant, causing altered movement patterns. This has been referred to as synergistic dominance. For example, in the case where a client sits for long periods the hip flexors become short and tight, which causes a shutting down or inhibition of the gluteal muscles (reciprocal inhibition and neural insufficiency). Since the gluteal muscles are no longer working correctly the body will begin to recruit the hamstrings (synergistic dominance) and the low back muscles to assist the gluteal muscles in hip joint extension, leading to postural and movement pattern dysfunction.
In a therapy exercise program the short/tight muscles are released by stretching and movement techniques that include micro control movements, strengthening and lengthening exercises such as on the Pilates Reformer.
The fascia is released through myofascial release techniques and trigger point therapy. Self-myofascial release (SMR) techniques (foam rollers, tennis balls) activate the nervous system sensory receptors in releasing muscle tension through autogenic inhibition. This reflex activates the golgi-tendon organs forcing the muscle’s stretch reflex to be inhibited, releasing muscle tension. It has the added benefit of releasing restrictive fascial tissue that surrounds the muscle component.
i.e. in the case described above of synergistic dominance, initially the corrective exercise specialist would prescribe stretching exercises for the iliopsoas such as push back on the reformer, rather than strengthening exercises for the gluteal muscles. By increasing the length of the hip flexors, it is possible to improve the activation of the gluteal muscles followed by a more formal strengthening program for these muscles. A full body integrated strength and movement program can then be prescribed to strengthen the weak or atrophied muscles by recruiting all the functional muscles in the body in large muscle movement patterns. Compound or isolated agonist movement patterns can also be prescribed to recruit specific muscle groups or specific muscles that require strengthening.
The overall aim of rehabilitation is to reverse the effects of immobilization. Although immobilization is a necessary part of the healing phase of any injury, prolonged immobilization will lead to significant loss of muscle strength and endurance, flexibility, proprioception and co-ordination A rehabilitation program include: regaining muscle strength, power and endurance, regaining joint range of movement, regaining joint stability, regaining proprioception of the injured joint and limb, and regaining exercise specific skills. It is also necessary to address any postural, anatomical or biomechanical dysfunctions that may have contributed to the initial injury
To become a corrective exercise specialist, you require a deep knowledge of anatomy & physiology, biomechanics and corrective exercise techniques. A worthwhile area of work and one that can increase your reputation and make you stand out from the crowd.
If you are interested in becoming a mat exercise therapist or a reformer exercise therapist why not book your level 4 Pilates Reformer course, Level 4 Mat Pilates course or your Exercise Therapy Course.